Austrian researchers are convinced that quantitative 3D measurements of meniscal position on MRI may open the door to a better understanding of knee pain in patients with osteoarthritis (OA).
In a pilot study of 53 patients with the same radiographic OA grade in both knees but only frequent pain in one, a team of researchers team led by Andrea Wenger of Paracelsus Medical University in Salzburg, Austria, found that extrusion of the meniscal body had a relationship with knee pain. They published their findings online in European Radiology on 14 August.
Seeking to explore the relationship between pain and quantitative measures of the meniscus in knees with the same radiographic OA grade, the team used clinical and imaging data from the Osteoarthritis Initiative to evaluate both knees of the same patient.
They specially sought to determine if knees with frequent pain display greater meniscal extrusion and whether knees with frequent pain display differences in meniscal size compared with contralateral knees with no pain.
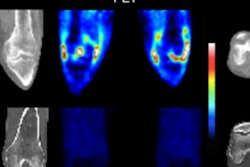
In the 19 men and 34 women that were included in the study, image analysis was performed using the public-use MRI dataset 0.E.1 acquired at 3-tesla on a Magnetom Trio (Siemens Healthcare) with a quadrature transmit-receive knee coil (USA Instruments). Coronally reconstructed double echo steady-state sequence with water excitation (corMPR DESSwe MRI: reconstructed slice thickness = 1.5 mm, in-plane resolution 0.37 × 0.7 mm interpolated to 0.37 × 0.37 mm) were utilized to analyze the tibial plateau and menisci.
In addition, two-dimensional coronal intermediate-weighted turbo spin-echo (IW.TSE) images (slice thickness = 3 mm interpolated to 1.5 mm, in-plane resolution 0.37 × 0.46 mm) were used to assist in the delineation of the surfaces in the corMPR DESSwe sequence. Blinded to the clinical status of the knees, two experienced musculoskeletal radiologists also used the IW.TSE images to determine lesion scores of the menisci in consensus.
Following manual segmentation using specialized software (Chondrometrics), 3D reconstructions of the segmented surfaces were completed for each compartment, and quantitative measurements were performed to compute coverage of the tibial plateau of the meniscus, meniscal size, meniscal bulging, meniscal position relative to the tibial plateau, as well as mean and maximum meniscal extrusion.
The researchers found that the medial meniscus covered 5% less of the tibial plateau and displayed 15% greater extrusion of the body in painful than in painless knees (p < 0.05). In addition, the external margin of the lateral meniscus showed 22% greater extrusion of the body in painful knees (p = 0.03). However, no significant difference was found in the position of its internal or tibial coverage.
The team also found that medial or lateral extrusion ≥ 3 mm was found in 23 painful knees, compared with 12 painless knees (p = 0.02). They did not uncover any significant association between meniscal size and knee pain.
"Extrusion of ≥3 mm (in the central five slices) was more frequent in painful than in contralateral painless knees, and more frequent in [Calculated Kellgren-Lawrence grade (cKLG)3] than in cKLG2 knees," the authors wrote.
In discussing their results, the authors noted that quantitative outcomes computed from the tibial surface and meniscal segmentation are not intended to replace semiquantitative scoring of the meniscus.
"Instead, they should be considered as a complementary assessment of tibial coverage, meniscal size, and meniscal position, which provide challenges in the subjective scoring of 2D images," they wrote. "Also, given its cost and complexity, the method is targeted at research studies exploring the pathophysiology of knee OA, but not at clinical diagnostics."
Further studies will need to confirm these findings and explore whether and to what extent meniscal extrusion is involved in the causation or mediation of knee pain in OA.
"If the current findings can be replicated, further studies will have to explore whether meniscal extrusion is causing pain, whether it is involved in mediating pain, or whether it is simply an 'innocent bystander' in this relationship," they wrote.