
Video capsule endoscopy (VCE) surpasses CT enterography and CT enteroclysis in detecting flat, small bowel lesions, but retrospective VCE and CT enterography findings in obscure bleeding need further evaluation, and an unbiased comparison of the two procedures is still needed.
These are the key findings of an ongoing research program led by one of Europe's leading gastrointestinal imaging specialists, Dr. Philippe Soyer, chairman of the department of radiology, interventional imaging and nuclear medicine at Hôpital Lariboisière in Paris.
"The question that remains unanswered is to determine to what extent CT enterography or CT enteroclysis and VCE are complementary and not competing techniques," he wrote in an editorial published online by European Radiology on 23 March. "Although some answers can be found in the literature published to date, this should be further evaluated by outcome-based, unbiased, large, and well-designed prospective studies."
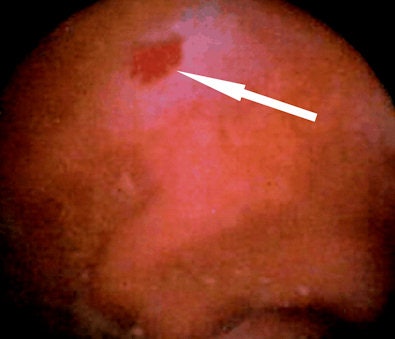 Video capsule endoscopy findings in a 72-year-old woman with obscure gastrointestinal bleeding. Whereas video capsule endoscopy reveals flat, vascular lesion of the distal ileum (arrow), CT enteroclysis failed to depict the vascular abnormality due to limited contrast resolution. Detection of flat, vascular lesions is a well recognized limitation of CT enteroclysis, and is the area in which video capsule endoscopy is markedly superior to CT enterography and CT enteroclysis. All images courtesy of Dr. Philippe Soyer.
Video capsule endoscopy findings in a 72-year-old woman with obscure gastrointestinal bleeding. Whereas video capsule endoscopy reveals flat, vascular lesion of the distal ileum (arrow), CT enteroclysis failed to depict the vascular abnormality due to limited contrast resolution. Detection of flat, vascular lesions is a well recognized limitation of CT enteroclysis, and is the area in which video capsule endoscopy is markedly superior to CT enterography and CT enteroclysis. All images courtesy of Dr. Philippe Soyer.Further studies must be conducted on CT enterography and CT enteroclysis in patients with occult obscure gastrointestinal bleeding (OGIB), and he favors direct comparisons with VCE and newer enteroscopy techniques, such as double balloon and spiral enteroscopy, and valid confirmation of the positive and negative findings.
CT enterography has major limitations in the evaluation of OGIB, according to Soyer. This is because vascular abnormalities account for 80% of OGIB, and especially angiodysplasia, which accounts for 50-60% of OGIB, whereas small bowel tumors are found in only 1.6% to 2.4% of patients undergoing VCE.
"VCE allows direct visualization of the small bowel mucosa and has a high sensitivity for the detection of flat lesions such as ulcers, angiodysplasias, or arteriovenous malformations, which are lesions beyond the reach of the best CT resolution available," he noted. "VCE shows ulcers and angioectasias that are not visible at CT enteroclysis. A large number of papers have showed that among the variable causes of OGIB, the one most commonly missed at CT enterography was small-bowel angioectasia."
At many centers, CT enterography is used instead of CT enteroclysis because it is better tolerated by the patient and performed more rapidly, but Soyer finds this approach unacceptable. Patients with OGIB should benefit from the best test available, and not from the most acceptable one. Should the same test combine both qualities, it can be selected, but if such a test does not exist, the most accurate one should be chosen. At this time there is no crystal-clear answer, and this should stimulate further studies, he stated.
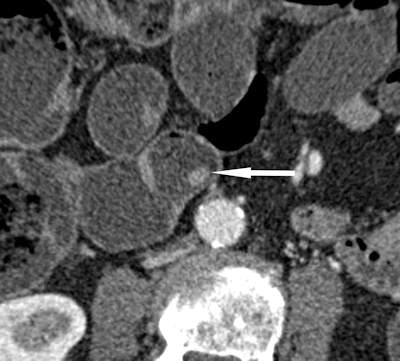 Small, benign polyp (arrow) of the jejunum measuring 6 mm in diameter is shown in an 84-year-old man who was investigated for obscure gastrointestinal bleeding. The lesion is detected with CT enteroclysis, with a high degree of confidence, whereas video capsule endoscopy failed to reveal the lesion.
Small, benign polyp (arrow) of the jejunum measuring 6 mm in diameter is shown in an 84-year-old man who was investigated for obscure gastrointestinal bleeding. The lesion is detected with CT enteroclysis, with a high degree of confidence, whereas video capsule endoscopy failed to reveal the lesion.Currently, two different diagnostic approaches to OGIB exist. The first is based on the use of CT enterography as an initial test only in patients with contraindications for VCE and in those with a suspected small bowel stricture or tumor. The second suggests that the role of CT enterography may be expanded to a first-line test in a broader population of patients.
"It is clear that CT enterography or CT enteroclysis and VCE are not competing but complementary techniques, the limitations of one being overcome by the advantages of the other," Soyer pointed out. "Results from the most recent literature suggest a complementary role for CT enterography or CT enteroclysis and VCE in the evaluation of patients with OGIB. However, because economic pressures favor the use of less expensive strategies, the two tests will not be performed routinely in the same patient. The question lies in deciding when one of these two approaches is the most appropriate."
Soyer and his colleagues are now developing virtual enteroscopy and cardiac imaging. His other main field of interest is abnormal placentation with conservative treatment, including pelvic embolization.
Further Reading
Khalife S, Soyer P, Alatawi A, Vahedi K, et al. Obscure gastrointestinal bleeding: Preliminary comparison of 64-section CT enteroclysis with video capsule endoscopy. Eur Radiol. 2011;21(1):79-86.



















