Patients with Middle East respiratory syndrome (MERS) have a unique presentation that clinicians are learning to recognize -- and medical imaging plays a role in both diagnosing and following up cases, according to researchers from Saudi Arabia in a new paper in Annals of Internal Medicine.
The MERS coronavirus (MERS-CoV) was isolated for the first time in September 2012 in a patient from Saudi Arabia who presented with acute pneumonia and renal failure. Since then, 170 confirmed cases of infection and 72 deaths have been reported to the World Health Organization.
The goal of the new study from lead author Dr. Yaseen Arabi, of the King Saud bin Abdulaziz University for Health Sciences, and colleagues was to shed light on the disease by studying particular cases of MERS (Ann Intern Med, January 28, 2014).
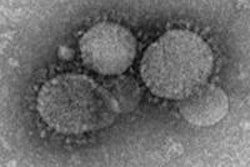
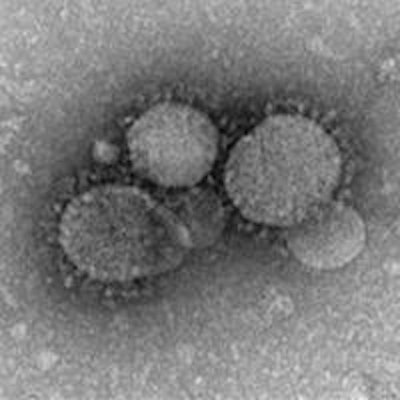
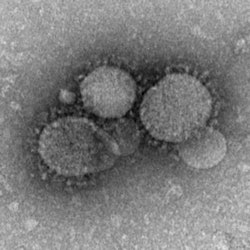 MERS-CoV as seen by negative stain electron microscopy. Image courtesy of the U.S. Centers for Disease Control and Prevention.
MERS-CoV as seen by negative stain electron microscopy. Image courtesy of the U.S. Centers for Disease Control and Prevention.Several clinical features of MERS-CoV infection resemble the infection caused by the severe acute respiratory syndrome coronavirus (SARS-CoV). However, the authors noted some important differences, including the fact that all patients with MERS-CoV had underlying comorbid conditions, such as asthma, diabetes, renal failure, cardiac disease, recent surgery, or heart failure. This strongly suggests that patients with such conditions are susceptible hosts.
However, even as knowledge about the virus is increasing worldwide, data on critically ill patients infected with MER-CoV are limited, the group noted.
Cases in Saudi Arabia
For the study, the researchers looked at the clinical course and outcomes of 12 patients with confirmed or probable infection from three intensive care units (ICUs) at two tertiary care hospitals in Saudi Arabia. One ICU was located at King Abdulaziz Hospital in Al-Ahsa, and two ICUs -- a medical/surgical ICU and a cardiac ICU -- were at King Abdulaziz Medical City in Riyadh.
Since the virus was first identified, healthcare facilities in Saudi Arabia have implemented guidelines for testing and screening for MERS according to directives from the Saudi Ministry of Health. The current study included all cases encountered from December 2012 through August 2013.
Infection was first suspected in patients presenting with acute respiratory illness and chest radiographs suggestive of pneumonia and acute respiratory distress syndrome, especially if the patient required ICU admission.
For their analysis, the authors included all patients admitted to ICUs with confirmed or probable MERS-CoV infection. They collected data on demographic characteristics, contact history with a confirmed case of MERS, underlying comorbid conditions, presenting symptoms, and radiographic findings.
During the nine-month study period, 114 patients were tested for MERS-CoV infection, and of these, 10 patients were confirmed while one was a probable case. Eight of the cases were community-acquired, and three occurred in patients in the cardiac ICU who were part of a healthcare-associated cluster. While three healthcare workers who were working without personal protective equipment were exposed, only one worker who had asthma became severely ill. The median age of the patients was 59 years (range, 36-83 years).
The presenting symptoms of these critically ill patients were mainly shortness of breath, cough, and fever; symptoms of upper respiratory tract infection were infrequent.
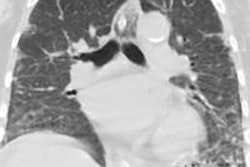
Acute severe hypoxemic respiratory failure was prominent, and all patients required invasive mechanical ventilation. Before intubation, five patients had received a failed trial of noninvasive positive-pressure ventilation. Chest radiography at the time of intubation showed airspace changes ranging from unilateral lobar to bilateral diffuse movement, and chest CT performed in three patients confirmed the same patterns.
The role of imaging
"Chest x-ray is needed for the initial evaluation and in the follow-up of critically ill patients with MERS-CoV," Arabi said in an interview with AuntMinnie.com. "It shows unilateral or bilateral infiltrates."
Radiologists should be especially alert to the condition when assessing certain patients, he added. The important take-home messages for radiologists are that they should consider the patient's travel history and take any necessary infection control measures.
"The disease should be suspected in patients residing in affected countries or returning travelers from these countries," he said. "If suspected, appropriate infection control measures must be taken to prevent transmission."
So far, MERS-CoV infection has been reported mainly in Saudi Arabia, with almost 80% of cases emerging from there, Arabi said. Other affected areas include Qatar, United Arab Emirates, Jordan, France, Italy, Kuwait, Oman, Tunisia, and the U.K.
Risk to healthcare personnel?
The authors cautioned that even though transmission of the virus to healthcare workers seems rare, human-to-human transmission does occur with unprotected exposure.
"Therefore, there is a concern that MERS-CoV may become highly infectious to humans with sustained human-to-human transmissibility," they wrote. "In such an event, along with the high pathogenicity of the virus, MERS-CoV will become a major public health threat worldwide."
They called for an urgent collaborative study to examine therapeutic options, such as convalescent plasma or ribavirin, interferon, or other drugs.
In an accompanying editorial in the journal, Dr. Trish Perl, from Johns Hopkins University and Bloomberg School of Public Health, and co-authors wrote that while "an intensive search for antivirals continues, a gap remains between this serious disease and effective therapy."
They noted that analysis to date suggests MERS-CoV infection does not yet have the potential to grow into a pandemic.
"However, we must keep in mind both the rapid evolution that occurred with SARS and the fact that it emerged in a much more densely populated region," they wrote. "Given the right environment and a crowded part of the world, MERS-CoV might propagate more readily."
They stressed that carefully designed case-control studies are essential to determine the exposures that lead to infection.
"As reported cases of MERS-CoV increase, we must not lose sight of the most important lesson of SARS: the value of transparency in reporting and of effective international collaboration in public health and research," Perl and colleagues concluded.