MANCHESTER - There's a great need to optimize and standardize patient care and imaging parameters to realize fetal MRI's potential, avoid unnecessary repeat examinations and improve image quality and efficiency, according to research presented at this week's U.K. Radiological Congress (UKRC).
"Fetal MRI is on the rise and can improve diagnosis of antenatal fetal conditions," noted Matt Fox, an MRI radiographer, and colleagues from the Imperial College Healthcare National Health Service (NHS) Trust in London. "More than half of our patients may complain of low back pain; optimal patient positioning ensured continuation of the MRI scan in order to collect useful diagnostic data."
Making use of hardware and software tools are essential to advance fetal imaging, and the development of faster MRI pulse sequences and other technological breakthroughs have contributed to the success of scanning random motion of the fetus and maternal breathing without the need for sedation.
However, the suboptimal use of equipment results in poor image quality; the optimal setup and use of equipment (coils and positioning aids) is necessary to prevent patient motion and reduce image artifacts. Correct patient positioning ensures comfort and reduces claustrophobia, and by appropriately selecting imaging parameters and adhering to safety guidelines, image quality can be optimized, they added.
"MRI of the developing fetus as a noninvasive in vivo imaging technique complimentary to ultrasound is increasing," Fox et al stated. "MRI of the fetal brain provides superior anatomical detail of the central nervous system (CNS) compared to ultrasound."
At their facility, fetal images are acquired using a 3-tesla Achieva system (Philips Healthcare). They use a 32-channel cardiac coil; these are not dedicated fetal coils, but they generate consistently reproducible high quality images when patient positioning is optimized relative to the coil.
To prepare the patient, they advise the following:
Ensure the patient has taken all necessary medication relevant to a pre-existing medical condition (e.g., diabetes, epilepsy). Check the patient for any metal before entering the scanner room.
Measure the patient's temperature before the MRI exam. Ensure the scanner fan is turned on and patient removes any head scarves to maximize heat dissipation.
Position the patient feet-first in the scanner in left lateral tilt at 45° or on left side to prevent inferior vena cava syndrome. Use positioning aids (foams pads, sand bags, wedges, pillows) to maximize patient comfort. Support lower back and legs.
Connect and adjust monitoring device for 02 saturation and heart rate. Visual monitoring of patient's condition in the scanner through a camera is advisable.
Use multichannel cardiac or body coil. Positioning coil must take into account maternal habitus (maximize patient comfort; firm, to keep it in place, but not too tight).
Fetal head position in pelvis (as close as possible to fetal head) to maximize signal-to-noise ratio. Give patient a buzzer to alert if in discomfort. Provide ear protection through head phones and earplugs.
Ensure Softone or any other noise reduction technique is enabled, when feasible. Ensure no crossing of arms and legs to prevent creating conductive loops; use padding in areas where patient's body might touch the bore (usually elbows). Interleave low and high specific absorption rate (SAR) scans to keep SAR within acceptable limits.
"Three-tesla provides increased signal-to-noise ratio, which can be traded off for higher resolution for cortical delineation at earlier gestations," the researchers noted. "Inhomogeneous radiofrequency distribution is caused by a variety of conductive and dielectric effects in tissue. While present at 1.5-tesla, these effects are exacerbated at higher field strength and typically manifest as image nonuniformity and shading. Sequences need to be carefully optimized as 3-tesla and advanced inhomogeneity techniques such as multitransmit need to be considered."
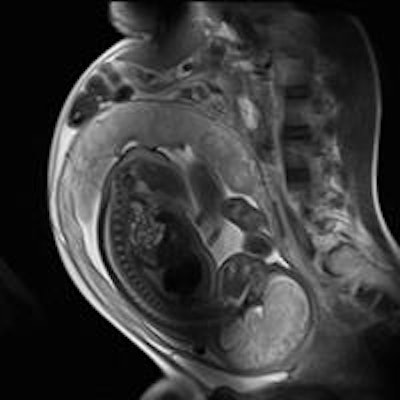
They recommend creating a dedicated optimized fetal brain imaging protocol, and they also think it is useful to create and save a fast fetal imaging protocol for claustrophobic patients; protocols should ensure full brain coverage in at least two imaging planes (transverse and sagittal), and images with single-shot T1 or Snapshot Inversion Recovery (SNAPIR)-like acquisitions as well as single shot T2 weighting (or half-Fourier acquisition single-shot turbo spin-echo-like acquisitions).
They recommend the following: repositioning coil after first survey scan, if required; using parallel imaging techniques to shorten scan time; using diffusion-weighted imaging and associated apparent diffusion coefficient maps if concerned about an acute brain injury (three directions with a b value of 500) to detect restricted diffusion in the fetal brain; using T2 gradient echo to detect blood products and hemorrhage, particularly in ventriculomegaly cases; and, considering fetal cine steady-state gradient echo acquisition for monitoring movements in utero, e.g. swallowing or to confirm fetal heart rate.
"Always plan on the most recent scan acquired; the assumption is that there is always some fetal movement," they advised. "Planning needs at least two different imaging planes -- ideally three -- one of which must be the survey, to avoid fold-over artifacts and cover all the required brain anatomy."
Images should be supplied for transverse, sagittal, and coronal plane planning, using a steeper angle than the standard one for the transverse plane. If significant motion occurs, a new survey scan is required, and image quality should be checked immediately. Also, check regularly if the patient feels OK and to inform them of the remaining scanning time, regular interaction is useful for anxious or claustrophobic patients, the researchers suggest. If the fetus is unsettled, try motion-resistant sequences such as dynamic or SNAPIR. If a break during the MRI scan is requested by the patient and the patient has changed position, then survey images and calibration scans need to be reacquired.
Editor's note: The image on our home page shows a sagittal half-Fourier acquisition single-shot turbo spin-echo (HASTE) scan used for planning further fetal images in other planes, and was taken at the Clinical Research Imaging Center, University of Edinburgh, U.K. Courtesy of Janet De Wilde, PhD, and Dr. Scott Semple.