It's essential to remember male breasts are not unique, with imaging features that are similar to those of the female breast. Use your knowledge of the female breast and apply it with a higher level of suspicion in the male breast, said researchers in Saudi Arabia and Canada.
Most male breast conditions encountered in daily practice are benign, such as gynecomastia and pseudogynecomastia. However, eccentric breast masses as well as solid and cystic masses in male patients are usually suspicious, and workup should be initiated if encountered, according to Dr. Shaza Alsharif, a radiologist at National Guard Health Affairs in Jeddah, Saudi Arabia, and colleagues.
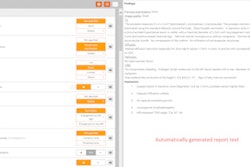
The group's objectives were to discuss the demographics of male breast tumors encountered in four institutions in Saudi Arabia and Canada, describe the diagnostic algorithm for evaluating male breast masses, review the imaging features of rare breast masses and the structures that can mimic male breast cancer, and discuss the impact of early and accurate diagnosis on the management options. They presented their experiences in an e-poster at RSNA 2015.
The male breast
The male breast can be affected by the same conditions affecting the female breast but with less frequency, probably due to lack of hormonal influence and consequently glandular subdevelopment. Most male breast masses are benign, with gynecomastia being the most common condition. Male breast cancer is rare, accounting for less than 1% of all breast cancers around the world. Gynecomastia is the most common male breast abnormality in daily practice.
In Saudi Arabia, the estimated incidence of breast cancer is between 0.9% and 2.13% of all cancers in men. In 2015, there were an estimated 220 new cases of breast cancer in men in Canada, resulting in 60 deaths (0.9 cases per 100,000). In 2015, there were an estimated 2,350 new cases of breast cancer in U.S. men, resulting in 440 deaths. The mean age at breast cancer diagnosis is 68 years old in Canada, with an 80% likelihood of living for five years after the diagnosis.
Currently, there are no established screening programs for men, because cancer prevalence is very low. The American Cancer Society estimates that more than 10% of male breast cancers are connected to BRCA mutations. Male BRCA carriers have an increased risk of developing breast cancer, among other cancers, and may benefit from screening. Men are often less likely to survive from breast cancer than women, because they are diagnosed with a more advanced stage of disease.
Other than gynecomastia, most male breast abnormalities are masses, followed by microcalcifications and asymmetries. The researchers did not encounter any distortions, which are extremely rare. In clinical practice, abnormalities not in the retroareolar location are usually suspicious and should be evaluated according to the BI-RADS lexicon, they added.
"If the abnormality is not gynecomastia, do ultrasound to further characterize the abnormality," they noted. "Ultrasound is usually sufficient for diagnosis and biopsy planning. Stereotactic-guided biopsy is usually not considered in the male breast due to the nature of the diseases encountered and technical difficulties."
Common male breast findings
Gynecomastia and invasive ductal carcinoma not otherwise specified are common occurrences; anything else is considered unusual.
Gynecomastia affects up to 65% of men and is of four types: florid gynecomastia (acute and reversible), dendritic gynecomastia (chronic and irreversible), diffuse pattern, and pseudogynecomastia.
- Florid gynecomastia appears with irregularly, retroareolar density. The pathology consists of irregular branching ducts with proliferation of epithelial cells and cellular and edematous stroma.
- Dendritic gynecomastia has small, flame-shaped retroareolar density. The pathology is hyalinized, sparsely cellular periductal stroma, and flat epithelial lining ducts.
- Diffuse pattern is usually the result of exogenous estrogen therapy and mimics the mammographic appearance of female breast cancer. The pathology is presence of lobules similar to the female breast.
- Pseudogynecomastia is difficult to distinguish from a normal male breast on mammography, and it manifests as breast enlargement on a clinical exam.
Papilloma is composed of finger-like fibrovascular cores covered by an epithelial and myoepithelial cell layer. On a mammogram, it appears as an isodense/hyperdense circumscribed retroareolar mass and is usually associated with gynecomastia. On ultrasound, it appears as an intraductal hypoechoic mass with intralesional or perilesional vascularity on color Doppler and can be associated with cystic changes and calcifications.
Pseudoangiomatousstromal hyperplasia (PASH) is stromal, myofibroblastic proliferation with slit-like pseudovascular spaces. It can be associated with up to 25% of gynecomastia cases. On a mammogram, it appears as isodense circumscribed masses. On ultrasound, it appears as circumscribed heterogeneous masses with vascularity in color Doppler. It also may recur after excision.
Hemangioma is a tumor or malformation of mature vessels. On a mammogram, it appears as circumscribed, superficial, isodense masses. On ultrasound, it appears as a circumscribed/noncircumscribed oval hypoechoic/hyperechoic mass. The researchers recommend excision, especially if the mass is palpable, to exclude well-differentiated angiosarcoma.
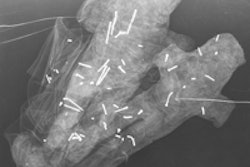
Pilomatricoma is a benign, cutaneous appendageal, adnexal neoplasm with hair follicle and matrix differentiation. In mammography, it appears as a circumscribed, superficial mass with microcalcifications. On ultrasound, it appears as a circumscribed, encapsulated, superficial, isoechoic/heterogeneous mass with posterior acoustic shadowing, bright foci, and a hypoechoic capsule. Wide local excision is the treatment of choice.
Lipoma is the second most common male breast mass along with pseudogynecomastia. It is composed of encapsulated, mature fat cells. On a mammogram, it appears as a circumscribed, fat-density mass with a thin, isodense capsule. If soft-tissue components or invasion are seen, suspect liposarcoma, the researchers wrote. On ultrasound, lipoma appears as a circumscribed, oval, slightly hyperechoic mass. A capsule also might be visible.
Angiomyxoma is composed of fibroblasts, myofibroblasts, and thick-walled blood vessels and presents as a painless, large, slow-growing mass. It's extremely rare in the breast. It is a locally aggressive, nonmetastasizing tumor with a high recurrence rate of up to 30%.
Angiolipoma is extremely rare in male breasts and is usually painless. In mammography, it appears as a circumscribed, encapsulated, fat-containing mass with soft-tissue densities representing branching small vessels more in a subcapsular location. On ultrasound, it appears as a circumscribed, hyperechoic mass.
Invasive papillary carcinoma is an invasive carcinoma that has predominantly papillary morphology (greater than 90%). It is more common in males than females; it's the second most common type of male breast cancer and represents 5% to 15% of male breast cancers. In mammography, it appears as a circumscribed, high-density mass. On ultrasound, it appears as a circumscribed, hypoechoic/complex mass with posterior acoustic enhancement. It usually has a better prognosis than carcinoma.
Noncircumscribed masses include primary breast cancer (ductal, lobular), Paget's disease, lymphoma, metastasis, myofibroblastoma, fat necrosis, and nodular faciitis.
Breast cancer accounts for less than 1% of cancers in males but 7% to 10% of cancers in BRCA-carrier males. Invasive ductal carcinoma not otherwise specified represents 85% of the cancers. Gynecomastia is associated with up to 50% of cases. Breast cancer usually presents as a hard, painless mass that can be fixed to the skin or nipple with associated nipple retraction, skin ulceration, and thickening with possible bloody nipple discharge. Palpable axillary lymph nodes are present in up to 50% of cases diagnosed with breast cancer in males.
Breast lymphoma is exceedingly rare in males and can be primary or secondary. On mammography, it is not specific and can be an equal or high-density mass. Also, imaging on ultrasound is not specific and can be hypoechoic/hyperechoic or a mixed echogenicity mass. The prognosis depends on the type of lymphoma diagnosed, the researchers wrote.
Breast metastasis is rare and accounts for 0.5% to 3% of cases. Out of those, 5% are in males. It is usually associated with disseminated metastatic malignancy. Nonmammary malignancy is usually lymphoma or leukemia in adults and rhabdomyosarcoma in children. Other malignancies metastasizing to the breast include lung, kidney, thyroid, stomach, and prostate cancers and melanoma.
Fat necrosis occurs after trauma and can be painful. It can simulate breast cancer acutely or have abscess imaging features. Chronic hematomas can develop calcifications. Fat-fluid levels can be seen, but vascularity should be absent in color Doppler. If fat necrosis is suspected, follow up in six weeks to be safe. If it's unchanged, a biopsy is indicated.
Myofibroblastoma is a rare, mesenchymal tumor that occurs in older males and presents as a painless mass associated with gynecomastia. On a mammogram, it appears as a circumscribed/noncircumscribed oval and is usually a dense mass. On ultrasound, it appears as a circumscribed/microlobulated hypoechoic mass. It can be followed or resected after core biopsy.
Ductal carcinoma in situ represents 5% to 11% of male breast cancers. It can be calcified or noncalcified. The most common subtype is papillary.
Cutaneous cyst is an epidermal inclusion cyst that is the third most common benign male breast mass. It occurs due to implantation of epidermal elements into the dermis due to previous trauma. In mammography, it appears as a circumscribed, isodense cutaneous mass. On ultrasound, it appears as a simple or complicated cyst in dermal location with a thin tract communicating to the skin.
Also contributing to this work were researchers at the King Faisal Specialist Hospital and Research Center in Riyadh, Saudi Arabia; McGill University Health Center in Montreal; and the University of Toronto in Canada.