New research from a large, public hospital in Russia has added fresh impetus to the creation of CT national reference values, and it may also lead to the closer involvement of Russia in international radiation safety initiatives.
 Dr. Valentin Sinitsyn is the new president of the Russian Society of Radiology. All figures courtesy of Sinitsyn and Dr. Elena Matkevich.
Dr. Valentin Sinitsyn is the new president of the Russian Society of Radiology. All figures courtesy of Sinitsyn and Dr. Elena Matkevich.According to Dr. Valentin Sinitsyn, professor of radiology and head of the radiology department at the Federal Center of Medicine and Rehabilitation, as well as president of ECR 2014, national diagnostic reference levels (DRLs) are essential because they enable medical authorities in each country to check that doses are in line with those in other countries; they make it possible to identify hospitals in which average dose falls above the national range; and they help to optimize technical standards for scanning.
"Establishing a reference will enable radiologists to set up acceptable technical parameters for CTs. For example, we know that 5-10 mm slice thickness is no longer acceptable for lung cancer screening," he told AuntMinnieEurope.com in an interview.
An important next step is to determine the standard dose for a patient with an average weight (70 kg to 80 kg) or body surface area (BSA).This would enable the comparison of radiation exposure dose levels between different hospitals in and outside Russia, added Sinitsyn, recently inaugurated as president of the Russian Society of Radiology (RSR).
"We shouldn't avoid CT for the right indications as it brings more benefits than harms. I am impressed by the capacity for decreasing radiation exposure while retaining image quality with new machines and algorithms -- even with lower-end scanners -- due to iterative image reconstruction techniques. However, radiologists need to know how to do this," he noted.
To date, no diagnostic reference levels have been analyzed or published for Russia, but the single site study by Sinitsyn and his colleagues may be the first step in an effort to establish a country-wide reference dose archive.
The new study comprises retrospective analysis performed using data from electronic patient records and PACS in the 450-bed Federal Center of Medicine and Rehabilitation in Moscow. Results were obtained for 1,626 patients (794 men, 832 women; age range 17 to 93) scanned during one year with one 40-slice and two 64-slice scanners. Volumetric CT dose index (CTDI) and dose-length product (DLP) were collected for each examination. The main findings can be seen in the tables below.
First presented at ECR 2015 by Dr. Elena Matkevich et al, the study showed the total number and structure of exams in a selected federal hospital between 2012 and 2013. Published as a paper in Russian in the journal Vestnik rentgenologii i radiologii (January-February 2016, Vol. 97:1, pp. 41-47), and with additional data, the study shows the structure and number of CT between 2012 and 2014. Both poster and paper also analyzed radiation exposure from CT per anatomical area and by scanner setting, and illustrated the feasibility of routine low-dose CT without the loss of diagnostic capacity.
The distribution of CT examinations according to anatomical regions scanned was as follows: brain (n = 329), chest (596), abdomen-pelvis (529), and chest-abdomen-pelvis (172). Data on the scanning parameters of each study were also collected and the mean CTDI and DLP were defined. Effective dose was calculated using the normalized coefficients according to the International Commission on Radiological Protection (ICRP) guidelines.
The mean DLP (M ± m) values (mGy*cm) with/without contrast medium, respectively, according to anatomical areas were: brain -- 1,021.8 ± 12.44/1,530.6 ± 101.20; chest -- 289.5 ± 6.91/659.2 ± 48.0; abdomen-pelvis -- 594.9 ± 23.71/2,177.7 ± 69.70; chest-abdomen-pelvis -- 736.2 ± 46.90/2,110.6 ± 106.90 mGy*cm.
The mean effective dose (M ± m) values (mSv) with/without contrast medium, respectively, according to anatomical areas were: brain -- 2.34 ± 0.03/3, 52 ± 0.23; chest -- 4.83 ± 0.11/11.02 ± 0.82; abdomen-pelvis -- 9.81 ± 0.40/36.6 ± 1.17; chest-abdomen-pelvis -- 12.41 ± 0.79/35.63 ± 1.81 mSv.
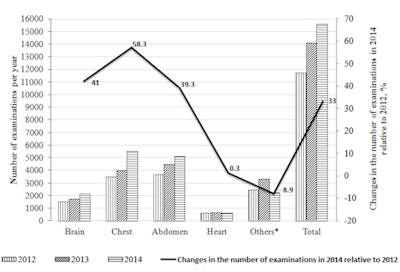 The number of CT examinations of the head, chest, abdomen, heart, and other areas in 2012-2014 in one state hospital.
The number of CT examinations of the head, chest, abdomen, heart, and other areas in 2012-2014 in one state hospital.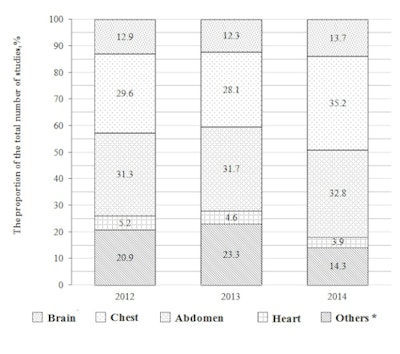 The ratio of CT examinations of the head, chest, abdomen, heart, and other areas in the overall structure of CT examinations in 2012-2014. Other * attributed CT study of the neck, pelvis, and extremities.
The ratio of CT examinations of the head, chest, abdomen, heart, and other areas in the overall structure of CT examinations in 2012-2014. Other * attributed CT study of the neck, pelvis, and extremities.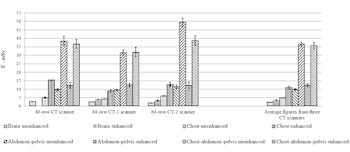
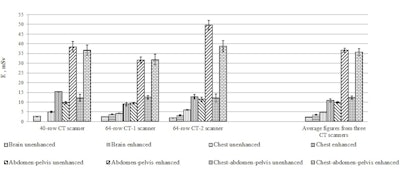
Mean E on one patient during one CT-examination, M ± m.
In terms of number, CT examinations in the hospital totaled 11,697 in 2012, 14,089 in 2013, and 15,557 in 2014 (fig.1), meaning that CT scans increased by 20.4% from 2012 to 2013 and by 33% from 2012 to 2014. The majority of the scans constituted CT of the brain, chest, and abdomen: in 2012 -- 73.8%; in 2013 -- 72.1%; and in 2014 -- 81.7% (fig.2).
In the final part of the study, Matkevich et al analyzed the image quality of low-dose CT examinations of the heart and coronaries, chest, and carotids. According to the authors, good diagnostic quality was maintained despite a reduction in radiation exposure, this achieved with decreased tube voltage (80 kV to 100 kV) and tube current in combination with iterative reconstruction (ASIR and MBIR).
Overall, the authors believe the results of this study exemplify CT dose values and distribution in a Russian federal hospital and these are comparable with international reference levels published by other groups. Also, the study confirms that low-dose CT is increasingly feasible for complex scanning that requires high image quality.
The authors note their statistics match the global trend of CT examination growth and increasing dose to the population from medical sources, with its potential risk of radiation-induced cancers and other diseases.
Sinitsyn is not surprised the study results were in line with other countries in Europe because Russian hospitals use the same scanners, follow the same protocols, and have the same strict guidelines governing CT indications and dose. The Moscow center has been performing low-dose coronary CT for five years, and with discussion about lung cancer screening and pediatric CT imaging increasingly in the spotlight, dose reduction has become a more urgent topic.
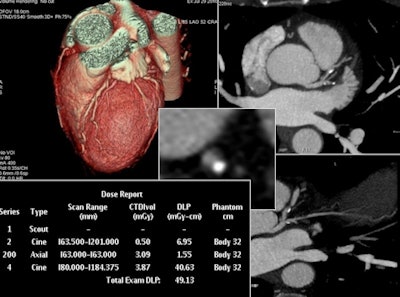 Low-dose CT for complex scanning is increasingly feasible, thanks to decreased tube voltage and current, in combination with iterative reconstruction, according to Sinitsyn. This reconstructed image from low-dose coronary CTA was achieved with reduced tube voltage of 80 kVp and automatic tube current modulation.
Low-dose CT for complex scanning is increasingly feasible, thanks to decreased tube voltage and current, in combination with iterative reconstruction, according to Sinitsyn. This reconstructed image from low-dose coronary CTA was achieved with reduced tube voltage of 80 kVp and automatic tube current modulation.He explained the department website regularly received letters from worried patients, particularly women, who typically discover postscan they were already pregnant when undergoing the exam. The Moscow group wanted to show that radiation exposure from CT in the hospital was compatible with levels in other countries and within acceptable limits.
"Patients are aware of the risks of CT scans," he said. "We need to show them that we are aware of them too, by doing everything we can to reduce dose," he said.
Sinitsyn promises the RSR will be more active on consolidating guidelines and promoting radiation exposure awareness. The plan is to create a registry network to collect and exchange data on doses between institutions and departments in Russia.
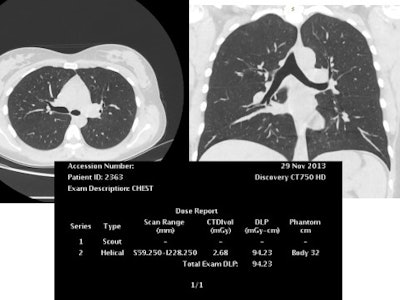 This reconstructed noncontrast CT image of the chest (lungs) was also achieved with reduced tube voltage of 80 kVp and automatic tube current modulation.
This reconstructed noncontrast CT image of the chest (lungs) was also achieved with reduced tube voltage of 80 kVp and automatic tube current modulation.A great enthusiast for iterative image reconstruction, he believes such techniques spell change for overall radiation reduction to patients and the wider population. However, he is aware that even when such tools are available, some doctors continue to choose standard protocols on advanced CT machines when low-dose protocols would be feasible.
"The number of CT exams in Russia is rising. Moreover we are also performing increasing numbers of combination CTs such as chest and abdomen, or pelvic abdomen scans, as well as oncological whole-body scans, which increase scan time and consequently dose. Often these combo scans are repeated in follow-up or therapy," Sinitsyn stated.
Each radiologist needs to think about how to reduce radiation without compromising image quality and life-saving diagnostic information, he said. "We have efficient tools to curb radiation dose, so let's use them."



















