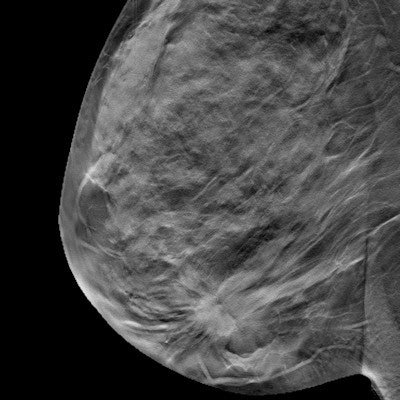
More and more clinical evidence indicates that using digital breast tomosynthesis (DBT) for breast cancer screening reduces recall rates and increases the detection of invasive cancers. Now another benefit of the technology is coming to the fore: Adding DBT to digital mammography helps breast imagers categorize lesions more accurately, according to research presented at ECR 2017.
More accurate lesion categorization -- for example, fewer BI-RADS 0 or 3 assessments, which tend to prompt callbacks -- leads to farther-reaching benefits, said presenter Dr. Flaminia Marzocca of the University of Rome.
"Patients' emotional distress is reduced, as well as financial and clinical costs to the hospital," she said. "And radiologists perform better."
Better BI-RADS
Marzocca and colleagues sought to assess the advantages of DBT in the assignment of BI-RADS categories and the management and follow-up of patients. The study included 214 patients, many of whom had dense breast tissue; some of the women had already had breast cancer (and therefore surgical treatment) or were symptomatic, Marzocca said.
Women who had undergone mammography less than one year before were excluded, as were those who had fatty or scattered fibroglandular breast tissue (according to the American College of Radiology's BI-RADS categories for density) or BRCA 1 or BRCA 2 mutations.
Between February 2014 and April 2015, each woman underwent two-view digital mammography, and then two-view digital mammography with one-view DBT. Two radiologists read the exams in two steps: digital mammography alone and digital mammography plus DBT. Each then assigned the exam a BI-RADS category. Patients with suspicious findings underwent fine needle or core biopsy followed by surgery, while those without suspicious findings were followed for one year.
Marzocca and colleagues calculated the percentages of BI-RADS categories for both technologies by single reader, and they evaluated interreader agreement for the classifications and any workup requests.
| Changes in BI-RADS categorization of mammography exams | ||
| Category | Digital mammography | Digital mammography + DBT |
| BI-RADS 0 (incomplete) and 3 (probably benign) | 56.7% | 7.9% |
| BI-RADS 1 (negative) and 2 (benign) | 25.7% | 61.9% |
| BI-RADS 4 (suspicious) and 5 (highly suspicious) | 17.5% | 30.1% |
Both readers' workup rates improved with the addition of DBT to digital mammography. Reader 1 went from an 85.9% workup rate with digital mammography alone to a rate of 52.8%, while reader 2 went from a 97.2% workup rate with digital mammography alone to a rate of 55.1%, Marzocca said.
Finally, the combination of digital mammography and DBT reduced the percentage of women called back from 91.5% with digital mammography alone to 53.9%.
This reduction in callbacks "means fewer supplementary exams and unnecessary biopsies," she said.
More effective
Marzocca noted that the study had a few limitations, including the fact that the researchers enrolled only women with dense breast tissue and those who had previously undergone surgery for breast cancer, as well as the small size of the cohort. But the findings still suggest that adding DBT to digital mammography makes mammography screening more effective, she told session attendees.
"We can affirm that [the DBT plus digital mammography combination] reduces false negatives and increases true positives," she said. "It also decreases the false-positive rate and therefore the number of callbacks. [All of these benefits] are good for patients, as well as the hospital."