
French researchers have shed new light on how to follow up patients with completely resected non-small cell lung cancer (NSCLC). CT may be a helpful yearly assessment tool in the longer term, but there is no proof the recommendation of a minimal biannual CT in the first two years after resection has any effect on overall survival, they found.
 Dr. Viginie Westeel, PhD, from Besançon.
Dr. Viginie Westeel, PhD, from Besançon.There was no difference in overall survival between patients who received CT scans as part of their follow-up and those who did not, according to study lead Dr. Virginie Westeel, PhD, head of thoracic oncology at the Jean Minjoz University Hospital in Besançon. She presented the results from the Francophone Thoracic Cancer Group (Intergroupe Francophone de Cancerologie Thoracique, IFCT-0302) trial.
She further suggested that performing chest CT in resected patients every three to six months, as recommended by many medical societies and clinical practice guidelines, may be of no value in the first two years after resection.
Following up
The multicenter study took place between 2005 and 2012 and included 1,775 patients with completely resected stage I-II-IIIA NSCLC who completed follow-up visits every six months for the first two years, and yearly until five years. Of these, 76% were male and the median age was 63.
Patients were randomized to a control follow-up (888 patients), that included clinical examination and chest x-ray, or an experimental follow-up (887 patients) that included the control protocol with the addition of thoraco-abdominal CT plus bronchoscopy (optional for adenocarcinomas). The primary endpoint was overall survival. The key findings are shown in the table below.
| Effect on survival of follow-up strategies in NSCLC patients | ||
| Control arm = 888 patients (clinical & x-ray follow-up) | Experimental arm = 887 (control follow-up protocol plus CT) | |
| Overall survival median | 99.7 months (8.3 years) | 123.6 months (10.3 years) |
| 3-year disease-free survival rate | 77.3% | 76.1% |
| 8-year overall survival rate | 51.7% | 54.6% |
After a median follow-up of eight years and 10 months, overall survival was not significantly different between the groups at a median of 99.7 months (8.3 years) in the control arm and 123.6 months (10.3 years) in the experimental arm. Three-year disease-free survival rates were similar at 77.3% and 76.1% respectively, and eight-year overall survival rates were 51.7% and 54.6%, respectively.
While there was a two-year difference between the median overall survival of 99.7 months in the control arm and 123.6 months in the experimental arm, the statistical comparison concerns the whole curves of the study data, which only diverge in the later parts, according to Westeel. Overall, the data curves from the two arms are not significantly different, she noted, adding that the trend toward better survival in the CT arm suggests patients might benefit from this approach in the long term.
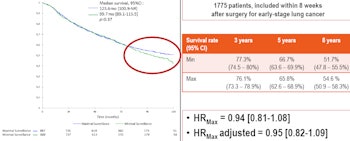
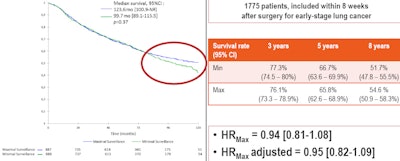
Overall survival data show no significant difference in survival between the minimal follow-up arm using the control protocol of clinical examination and x-ray (Min), and the maximum follow-up arm using the control follow-up protocol with CT (Max). The curves diverge in the later stage (circled in red), suggesting that CT follow-up may be of benefit to some patients in the longer term. All figures courtesy of Dr. Viginie Westeel, PhD.
At present, no further studies are planned and the group is analyzing the database and preparing the manuscript for publication.
"Most clinical practice guidelines recommend chest CT as part of the follow-up, but the level of evidence is low. There has been, until now, no randomized controlled study addressing this question," Westeel told AuntMinnieEurope.com.
"Our study does not demonstrate a significant benefit with CT-based follow up. Because there is no survival difference, both the control and the experimental follow-up protocols are acceptable. However, I would not consider doing chest CT every six months during the first two postoperative years anymore," she said, confirming that she will cease such requests in her own practice.
Future strategy
Whether yearly CT scans should start within the first two postoperative years or afterward should be investigated, she said.
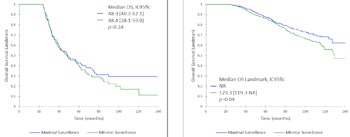
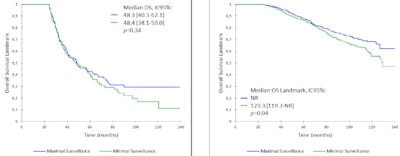
Exploratory analysis of survival comparison between arms for patients with (left) and without (right) recurrence at 24 months. An exploratory analysis revealed that patients who had a recurrence within two years had no benefit from CT. However, patients who experienced no recurrence or second primary cancer after two years might benefit from a CT-based follow-up.
Yearly CT exams beginning at one year after resection are closest to current clinical practice, and probably easier to organize in terms of patient adhesion, however it can be challenged with the risk of radiation exposure, Westeel noted. That said, she pointed to a significant proportion of patients with early stage NSCLC who develop second cancers between the second and fourth year after surgery: Early detection of these with CT beyond two years after resection could allow curative treatment. Therefore yearly CT-based surveillance may still be appropriate because of its potential for detecting second primary cancers.
"Patients who had experienced no recurrence or second primary cancer after two years might benefit from a CT-based follow-up," she said.
Because these patients are at high risk of second primary cancer, a low-dose CT scan, as recommended for screening, may be proposed, Westeel noted. However, she warned that for these patients at probable high risk of a second primary cancer, the optimal long-term surveillance strategy was not yet known.



















