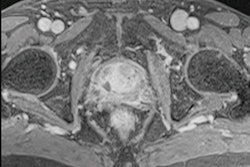
Multiparametric MRI (mpMRI) on 3-tesla scanners showed little advantage over 1.5-tesla imaging in a direct comparison in prostate cancer patients with total hip replacements. The German study was published on 11 September in the European Journal of Radiology.
German researchers compared mpMRI at both field strengths and observed no significant differences between the two in artifact severity and the overall diagnostic value of images. The finding is significant given that more patients are undergoing MRI prostate exams while hip replacements are expected to skyrocket.
"There was no significant difference between artifact severity in prostate mpMRI of patients with hip arthroplasty between 1.5T and 3T examinations," wrote first author Matthias Boschheidgen from the department of radiology at Dusseldorf University Hospital and colleagues.
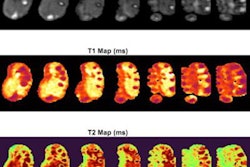
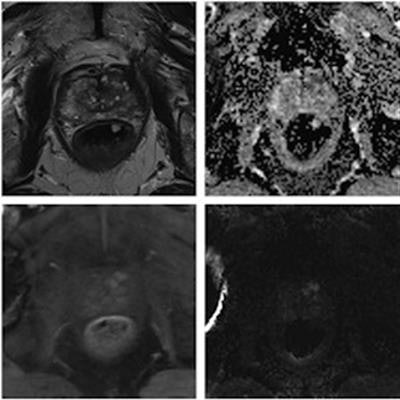
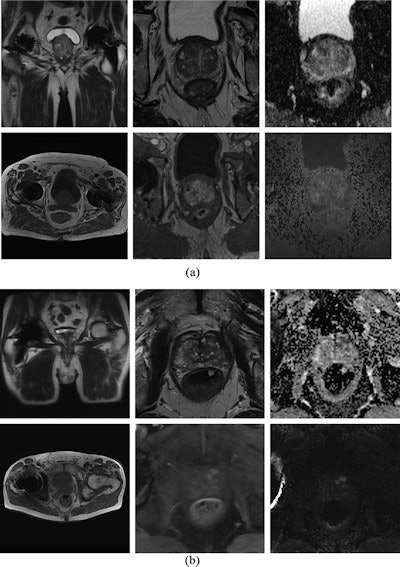 Diagnostic MRI at 1.5 tesla and 3 tesla. MpMRI without impairment of diagnostic value at 1.5 tesla (a) and 3 tesla (b). Top left shows localizer with little susceptibility artifacts caused by the total hip replacement. Top center: T2-weighted images. Top right: Apparent diffusion coefficient maps. Bottom left: T1-weighted images. Bottom center: T1 volumetric interpolated breath-hold examination (VIBE) for dynamic contrast-enhanced images. Bottom right: Diffusion-weighted imaging high b-values (b1800). Image courtesy of the European Journal of Radiology.
Diagnostic MRI at 1.5 tesla and 3 tesla. MpMRI without impairment of diagnostic value at 1.5 tesla (a) and 3 tesla (b). Top left shows localizer with little susceptibility artifacts caused by the total hip replacement. Top center: T2-weighted images. Top right: Apparent diffusion coefficient maps. Bottom left: T1-weighted images. Bottom center: T1 volumetric interpolated breath-hold examination (VIBE) for dynamic contrast-enhanced images. Bottom right: Diffusion-weighted imaging high b-values (b1800). Image courtesy of the European Journal of Radiology.MpMRI of the prostate has become a significant part in the detection and monitoring of prostate cancer, and the number of MRI examinations has increased significantly in the past decade. Meanwhile, total hip replacement is a common orthopedic operation in the developed world, with the rate predicted to double by 2035.
Artifacts due to total hip replacement can be severe enough to degrade MRI image quality and interfere with interpretation. Thus, effective imaging techniques to help limit image distortion and artifacts are essential, according to the authors.
In this retrospective multicenter study, the investigators compared results from 70 patients with hip replacements who underwent 1.5-tesla mpMRI prostate cancer exams (Magnetom Avanto fit, Siemens Healthcare) and 70 patients who had 3-tesla exams (Magnetom TIM Trio, Prisma or Skyra; Siemens Healthcare). The diagnostic mpMRI studies were evaluated by three readers with three, six, and 11 years of experience.
The overall diagnostic value and prostate imaging quality score (PI-QUAL) were assessed. Artifact severity in the localizer and mpMRI sequences (T2W, diffusion-weighted imaging, and dynamic contrast-enhanced imaging, or DCE) was scored on a three-point scale. The researchers analyzed correlations between diagnostic value and artifacts. The primary endpoint was the diagnostic value of mpMRI-scans at 1.5 tesla and 3 tesla.
Artifacts that impaired image quality substantially occurred at both field strengths in about 30% of patients, the authors found. Artifacts in all MRI sequences and in the localizer at 3 tesla correlated significantly with the diagnostic value, whereas T2-weighted sequences at 1.5-tesla were not as strongly correlated as in 3-tesla examinations, the researchers found.
Boschheidgen and colleagues observed a PI-QUAL score of less than 3 in 19 scans at 3 tesla and in 22 scans at 1.5 tesla; 39% of the scans at 1.5 tesla and 30% of the scans at 3 tesla exhibited excellent image quality with a PI-QUAL score of 5.
"Patients with [total hip replacement] showed similar artifact severity at both 1.5T and 3T scanners for prostate MRI examinations," the authors stated.
In addition, the authors noted an interesting finding -- the predictive value of the localizer for artifact severity. Results demonstrated that the extent of artifacts in the localizer correlated with the diagnostic value of subsequent MRI sequences.
"The knowledge and anticipation of artifacts may also reduce the number of unnecessary sequence repetitions and may save additional scanning time," they stated.
Ultimately, current European guidelines recommend both 1.5-tesla and 3-tesla MRI scanners as appropriate for mpMRI of the prostate. However, new approaches are in development to reduce artifacts and eventually may be available in clinical routine, the authors added.
"Patients with hip metalwork benefit from technical progress and new approaches that guarantee excellent diagnostic performance," the researchers concluded.