
Both radiologists and referrers are far too acceptant of and reliant on telephone interruptions as part of their workflow, a new U.K. study has found. What's more, the benefits of electronic order systems are not being realized, and change management is required in this area.
The findings come from a study performed at two hospitals that have modern order communication systems with linked electronic patient records. This means phone calls during reporting sessions to communicate urgent requests and reports are necessary only in exceptional circumstances, but interruptions still occur alarmingly often, according to Dr. Christopher Watura and colleagues in the imaging department at Imperial College Healthcare National Health Service Trust in London.
Telephone calls are one of the most frequent interruptions to reporting, and a call during the hour before completing a report may increase the chance of discrepancies by 12%, Watura told delegates at last month's U.K. Radiological Conference (UKRC) in Manchester.
To help better understand the characteristics of calls to the reporting rooms and identify potential changes to reduce interruptions, the group conducted an observational study over five working days (10 scheduled activity reporting sessions equivalent) in November 2016 at two large acute general teaching hospital reporting rooms covering conventional and interventional services where radiologists report studies and vet imaging requests.
Radiologists were asked to record all calls between 9 a.m. and 5 p.m. on an electronic form. They completed a total of 23 forms: four came from senior/consultant radiologists, eight from radiology specialty training year 1's (ST1s), six from ST2s, two from ST3s, one from ST4s, and two from ST5s or above.
Of the 288 phone calls recorded, 266 (92%) interrupted reporting. The callers were senior house officers (qualified specialist doctors below consultants) in 129 (45%) cases, registrars (middle-ranking doctors undergoing specialist training) in 51 (18%) cases, foundation year 1's in 32 (11%) cases, other staff in 62 (22%) cases, and consultants in 14 (5%) cases, Watura and colleagues noted.
 Source: Dr. Christopher Watura, presented at UKRC 2017.
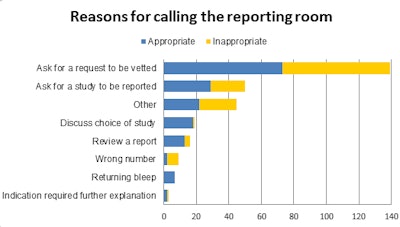
Source: Dr. Christopher Watura, presented at UKRC 2017.As shown in the figure, nearly half of the 288 calls (139 or 48%) were to ask for an imaging request to be vetted.
The purpose of another 50 (17%) comprised a request for a study to be reported, while 19 (7%) were to discuss the choice of study, 16 (6%) were to review a report, nine (3%) were the wrong number, seven (2%) were to return a bleep, 3 (1%) were to provide further explanation for a request in addition to the electronic form. For the remaining 45 (17%), the reason was listed as "other."
A total of 166 (58%) calls were deemed to be appropriate by the reporting radiologist, they added. Of the 122 inappropriate calls, 66 (54%) were to ask for a request to be vetted, 23 (19%) were classified as "other," and 21 (17%) were to ask for a study to be reported.
In all, 9,944 studies were performed over seven days between Monday and Sunday, with a rate of 2.9% (288 out of 9,944) in-hour calls per total number of studies performed.
"Due to time pressures on radiologists completing forms, our data underrepresents the total number of calls," Watura noted.
The large number of calls asking for requests to be vetted and studies to be reported -- over half of which were categorized as appropriate -- suggests that the benefits of an electronic order system are not yet being realized and changes are needed, he continued.
At Imperial College Healthcare, the actions being taken include a review of booking and vetting processes for inpatient and acute studies to reduce calls for vetting and a review of reporting triaging to cut down on calls for reports. Many calls for reports, however, are due to an outpatient reporting backlog (not recorded), which also could be improved by faster reporting turnaround times through increased resource allocation, the researchers concluded.



















