Multiparametric ultrasound, including contrast-enhanced ultrasound (CEUS), is an ideal diagnostic tool for penile traumatic injuries because it has a high resolution and is portable, safe, and widely available, prize-winning researchers reported at ECR 2023.
Penile trauma is a urological emergency that is often underdiagnosed, and it can have severe consequences, such as infarction or infection, according to Dr. Miguel Ángel Gómez-Bermejo, who is based at Hospital Universitario Ramón y Cajal in Madrid and was a European School of Radiology (ESOR) fellow at the King's College Hospital NHS Foundation Trust in London between September and December 2022.
"CEUS may help to delineate both cavernosal and extratunical hematomas, as they do not enhance after microbubble injection," explained Gómez-Bermejo and colleagues in an e-poster that received a cum laude award at ECR 2023. "CEUS improves the localization of tears of the tunica albuginea and could help to differentiate cavernosal tissue herniation from hematoma, as the former enhances."
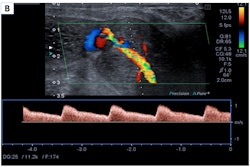
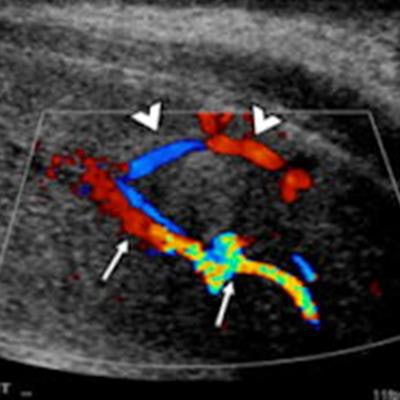
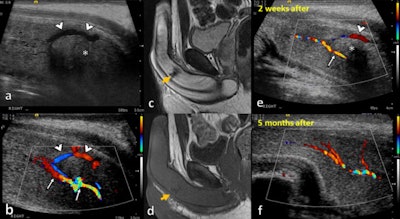 A 37-year-old man presented after a crush injury to the perineum with swelling and high-flow priapism. On ultrasound in a sagittal plane of the right cavernosal body at the base of the penis (a-b), there is an abnormal communication between the right cavernosal artery (thin arrows) and a prominent draining vein (arrowheads) consisting of an arteriovenous fistula. There is an associated cavernosal hematoma (asterisk). Two weeks later, an MRI scan without contrast was performed, showing an area of hypointensity both on T2-weighted imaging (c) and T1-weighted imaging (d) compatible with a late subacute-chronic hematoma. The arteriovenous fistula was embolized with Gelfoam (not shown). A follow-up ultrasound was performed two weeks later (e). It demonstrates persistence of the fistula, but with a decrease in the size of the hematoma (asterisk) and a reduction in the calibre and peak systolic velocity of the right cavernous artery (thin arrow). Five months later (f), the cavernosal hematoma and arteriovenous fistula had disappeared. All images courtesy of Dr. Miguel Ángel Gómez-Bermejo, Dr. Dean Huang, and Prof. Paul Sidhu.
A 37-year-old man presented after a crush injury to the perineum with swelling and high-flow priapism. On ultrasound in a sagittal plane of the right cavernosal body at the base of the penis (a-b), there is an abnormal communication between the right cavernosal artery (thin arrows) and a prominent draining vein (arrowheads) consisting of an arteriovenous fistula. There is an associated cavernosal hematoma (asterisk). Two weeks later, an MRI scan without contrast was performed, showing an area of hypointensity both on T2-weighted imaging (c) and T1-weighted imaging (d) compatible with a late subacute-chronic hematoma. The arteriovenous fistula was embolized with Gelfoam (not shown). A follow-up ultrasound was performed two weeks later (e). It demonstrates persistence of the fistula, but with a decrease in the size of the hematoma (asterisk) and a reduction in the calibre and peak systolic velocity of the right cavernous artery (thin arrow). Five months later (f), the cavernosal hematoma and arteriovenous fistula had disappeared. All images courtesy of Dr. Miguel Ángel Gómez-Bermejo, Dr. Dean Huang, and Prof. Paul Sidhu.Also, CEUS can increase the operators' confidence in confirming vessel patency and demonstrating active bleeding and pseudoaneurysms, and it can help to locate a dislocated penis and assess its viability.
What's the best technique?
Imaging allows a useful assessment of injuries for an easier decision on either surgical or conservative management, the authors explained.
"Ultrasound examination should be performed ideally with the patient supine while holding his penis' tip onto his abdomen. A supporting towel between the patient's thighs will help elevate the scrotum," they noted. "In a degloving injury, a careful ultrasound investigation using sterile gel and transducer covers is essential. Ultrasound is conducted using a linear transducer of 7 and 15 MHz."
Penile ultrasound should include longitudinal and transverse greyscale and Doppler color-flow images of the entire length of the penis, and if good visualization of the base of the penis cannot be obtained, a transperineal approach with the elevation of the testes should be considered, they continued.
"CEUS can be performed in patients with renal impairment and needs no prior laboratory testing," the researchers pointed out. "Ultrasound contrast agents are purely intravascular and the phospholipid shell is metabolized by the liver and the SF6 gas component is exhaled through the lungs. They have a low risk of adverse reactions compared to contrast agents used in CT and MRI."
The authors recommend a split-screen approach, with B-mode and CEUS images displayed side-by-side, allowing low mechanical index (MI) B-mode images to localize the area of interest, and they propose a dose of 4.8 ml of SonoVue/Lumason. A CEUS examination requires intravenous access for contrast administration, with a minimum calibre of 18-22-G, and prompt access to resuscitation equipment should be available.
The dynamic range should be wide if fine differences of enhancement are sought, or low to make the blood vessels stand out more brightly for addressing vascular injuries. A frame rate of more than 10 Hz/fps is useful for assessing active bleeding, but this comes at the expense of microbubble disruption. An MI that is too high will cause microbubble disruption, particularly in the near field, whereas an MI that is too low will lead to poor visualization of the far field. Take video clips for reevaluation and avoid prolonged scanning of the same area, the researchers advised.
Some typical findings
Cavernosal hematomas usually result from injury to the subtunical venous plexus or smooth-muscle trabecula secondary to compression of the penis shaft against the pelvic bones, and they are often bilateral and can be associated with penile fractures and arterial injuries with high-flow priapism, the authors wrote.
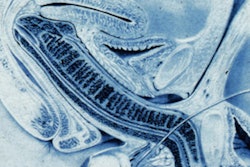
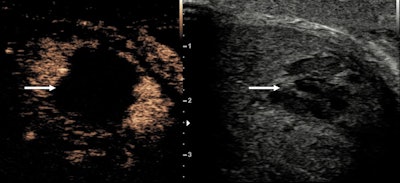 A hematoma within the corpora cavernosa, with contrast ultrasound examination confirming the avascular nature of the lesion, and the clear size and extent (arrows).
A hematoma within the corpora cavernosa, with contrast ultrasound examination confirming the avascular nature of the lesion, and the clear size and extent (arrows).Extratunical hematomas can be superficial or deep to the Buck fascia, depending on the site of involvement of the penile veins, and they can be associated with an arterial lesion (such as an arteriovenous fistula) or thrombosis of the superficial and deep dorsal penis veins.
"The B-mode appearance of a penile hematoma can vary with its age, being hyperechoic in the acute phase and cystic with septations in chronic stages. In the long-term, fibrosis can be developed, appearing as an ill-defined echogenic abnormality," the authors noted, adding that on CEUS, a penile hematoma appears as a non-enhancing area, and it allows a confident diagnosis and a better delineation of the hematoma.
Patients with penile fractures often report hearing a cracking sound and sharp pain followed by rapid detumescence, swelling, and deformity of the penis (described as an "aubergine deformity"). Penile fractures consist of a tear in the tunica albuginea, typically in the proximal or midshaft of the erect penis. They are urologic emergencies and require immediate surgical exploration, according to the researchers.
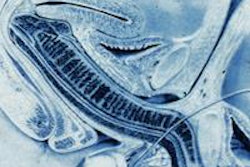
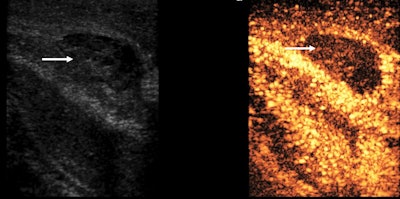 A penile fracture with an avascular hematoma (arrow) on the contrast ultrasound examination, lying outside the tunica albuginea of the corpora cavernosa.
A penile fracture with an avascular hematoma (arrow) on the contrast ultrasound examination, lying outside the tunica albuginea of the corpora cavernosa.Concomitant injury to the penile urethra occurs in approximately 10% to 20% of cases and should be suspected if blood is found within the urethral meatus or if the cavernosal injury is bilateral. A retrograde CEUS-urethrogram can be confirmatory, they stated.
In some cases of penile trauma (e.g., a traumatic arteriolacunar fistula), CT can be of value.
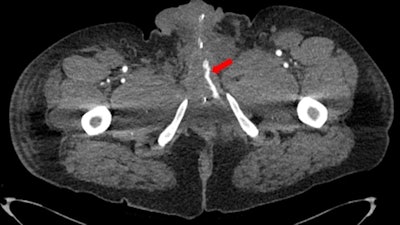 CT scan shows a traumatic arteriolacunar fistula, with the left cavernous sinus exhibiting early enhancement (indicated by red arrow) compared to the right.
CT scan shows a traumatic arteriolacunar fistula, with the left cavernous sinus exhibiting early enhancement (indicated by red arrow) compared to the right."Miguel was our ESOR Scholar this year and it was his project that won the prize at ECR 2023," Prof. Paul Sidhu said. "King’s has had the largest number of ESOR scholars at 45, and we were awarded a appreciation certificate this year."
Dr. Dean Huang, a consultant radiologist at King's, agrees. "Collaborating with our ESOR scholars, who represent the finest of future radiologists in their respective countries, has been a rewarding experience. Much credit goes to Dr. Annamaria Deganello for administering the ESOR fellowship programme," he added.
For more cases and a full description of the optimum use of ultrasound, please view the whole ECR 2023 poster on the EPOS section of the congress organizers' website.