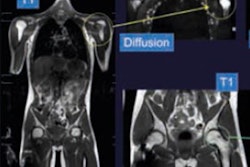
The careful evaluation of the immediate area around soft-tissue sarcomas with MRI before, during, and after neoadjuvant chemotherapy can help clinicians alter cancer treatment, if necessary, and better predict a patient's prognosis based on certain early indicators, according to a French study published online on 5 November in the European Journal of Radiology.
More specifically, stable or increased contrast-enhanced edema and an excessive accumulation of cancer in adjacent tissue -- known as diffuse infiltrative growth pattern -- detected on baseline and midtreatment MRI correlated with reduced disease-free survival among patients with soft-tissue sarcomas. When stable or increased contrast-enhanced edema was present on MRI after therapy, a patient's chance of overall survival and disease-free survival both worsened.
"Surrounding tissues of soft-tissue sarcoma during neoadjuvant chemotherapy should be carefully evaluated, as they may steer treatment efficacy and patient prognosis," wrote lead author Dr. Amandine Crombé, a radiologist from the Bergonié Institute in Bordeaux, and colleagues. "The ability to anticipate poor responses during neoadjuvant chemotherapy course may help to adjust treatment."
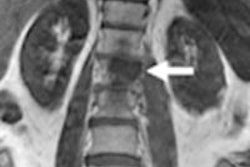
MRI is known to detect a wide range of abnormalities in tissue surrounding soft-tissue sarcomas, which could develop into high-grade tumors beyond the primary cancer site. The presence of infiltrative growth pattern and increased edemas have been associated with high-grade soft-tissue sarcoma, which naturally can lead to adverse consequences for patients.
"Surrounding tissues of soft-tissues sarcomas demonstrate various aspects at baseline and during treatments," Crombe and colleagues noted, "but their relevance to predict histological response and prognosis is poorly understood."
The researchers' goal was to evaluate the area around the sarcoma using MRI to record pretreatment conditions, the efficacy of neoadjuvant chemotherapy, and correlate patient response with their outcomes to determine how these factors might predict survival.
In this study, 57 patients (median age 58, range, 31 to 77) with newly diagnosed, locally advanced, high-grade soft-tissue sarcomas underwent contrast-enhanced baseline MRI scans on a 1.5-tesla system (Magnetom Aera, Siemens Healthineers) prior to treatment and again after two or three cycles of neoadjuvant chemotherapy. In addition, 37 patients underwent a preoperative contrast-enhanced MRI after five or six treatment cycles, which concluded their therapy.
When Crombé and colleagues compared baseline and MRI scans, and abnormalities around the soft-tissue sarcomas, changes in infiltrative growth pattern and stable or increased edema contributed to statistically significant reduction in disease-free survival.
| Prognostic value MRI scans at baseline & midtreatment | |||
| Infiltrative growth pattern | Stable or increased edema | ||
| Disease-free survival | Hazard ratio | 3.72 | 2.80 |
| p-value* | 0.040 | 0.040 | |
In addition, MRI scans performed after treatment showed stable or increased edema was a statistically significant predictor of both lower overall survival and disease-free survival.
| Prognostic value of MRI scans at end of treatment | ||
| Stable or increased edema | ||
| Overall survival | Hazard ratio | 2.80 |
| p-value* | 0.40 | |
| Disease-free survival | Hazard ratio | 4.98 |
| p-value* | 0.006 | |
The findings "emphasize the importance of MRI analysis of soft-tissue sarcoma's tissue periphery," the researchers concluded. "Further studies are needed to confirm these results and investigate prospectively soft-tissue sarcoma periphery with standardized multimodal imaging and pathological protocols."